Contrary to what has been generally assumed so far, a severe course of COVID-19 does not solely result in a strong immune reaction – rather, the immune response is caught in a continuous loop of activation and inhibition. Experts from Charité – Universitätsmedizin Berlin, the University of Bonn, the German Center for Neurodegenerative Diseases (DZNE), the Helmholtz Centre for Infection Research (HZI) and the German Center for Infection Research (DZIF), along with colleagues from a nationwide research network, present these findings in the scientific journal Cell.
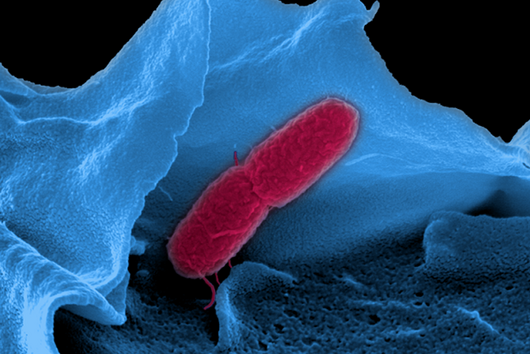
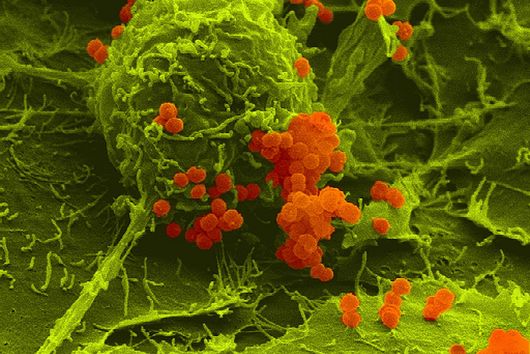
Most patients infected with the coronavirus SARS-CoV-2 show mild or even no symptoms. However, 10 to 20 percent of patients develop pneumonia during the course of COVID-19 disease, some of them with life-threatening consequences. "There is still not very much known about the causes of these severe courses of the disease. The high inflammation levels measured in those affected actually indicate a strong immune response. Clinical findings, however, rather tend to indicate an ineffective immune response. This is a contradiction," says Joachim Schultze, Professor at the University of Bonn and research group leader at the DZNE. "We therefore assume that although immune cells are produced in large quantities, their function is defective. That is why we examined the blood of patients with varying degrees of COVID-19 severity," explains Leif Erik Sander, Professor of Infection Immunology and Senior Physician at Charité’s Medical Department, Division of Infectious Diseases and Respiratory Medicine.
High-precision methods
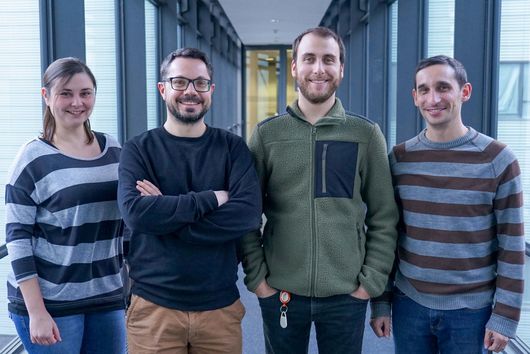
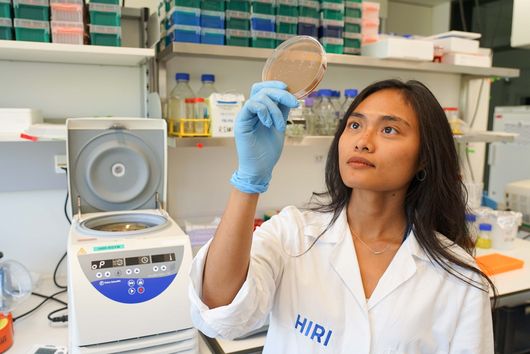
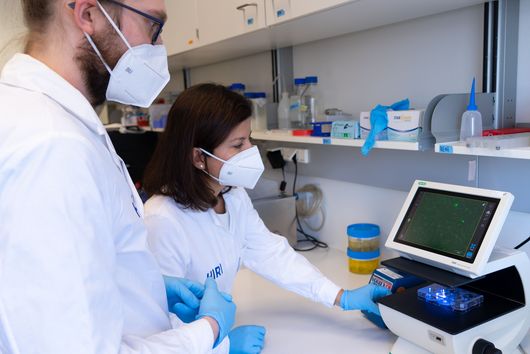
The study was carried out within the framework of a nationwide consortium – the "German COVID-19 OMICS Initiative" (DeCOI) – meaning that the analysis and interpretation of the data was spread across various teams and sites. Joachim Schultze was centrally involved in coordinating the project. The blood samples were derived from a total of 53 patients with COVID-19 from Berlin and Bonn, whose course of disease was classified as mild or severe according to the World Health Organization classification. Blood samples from patients with other viral respiratory tract infections as well as from healthy individuals served as important controls.
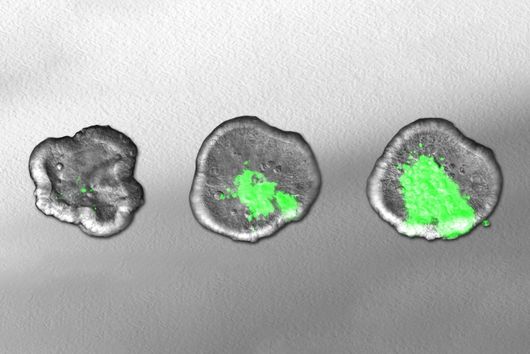
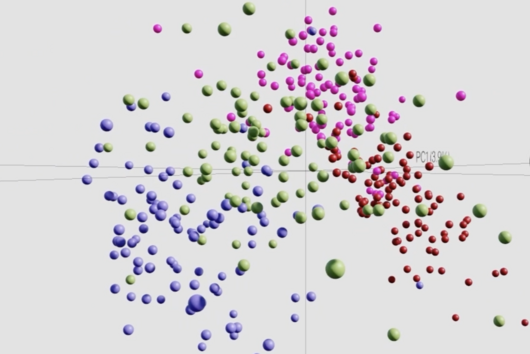
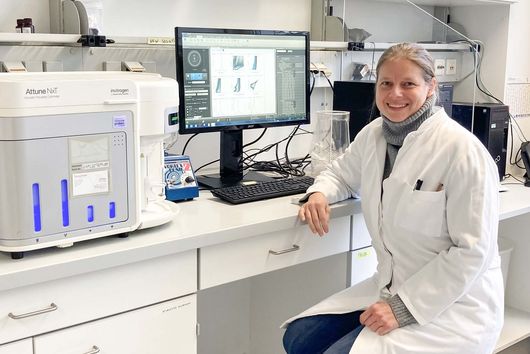
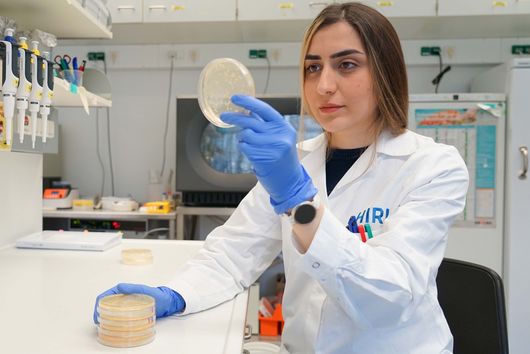
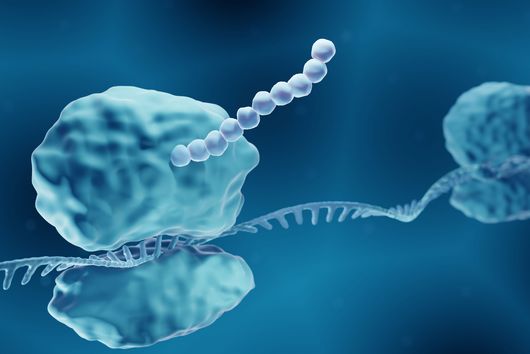
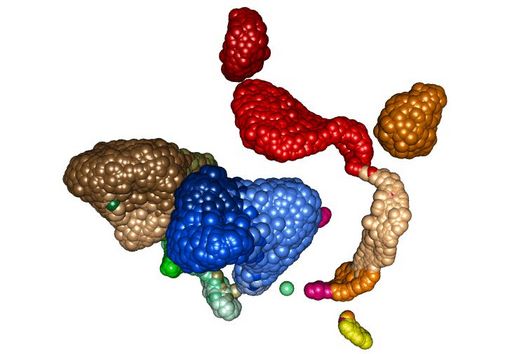
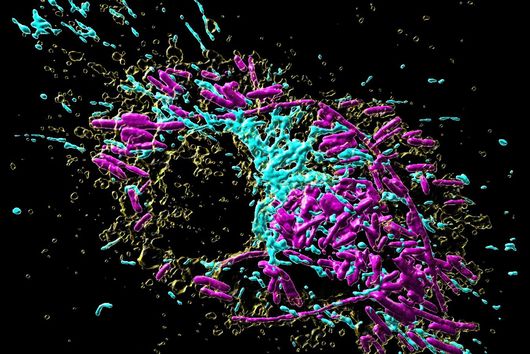
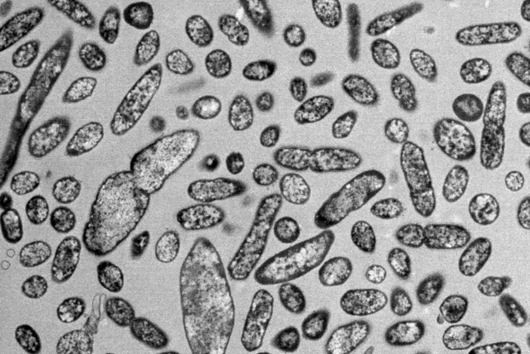
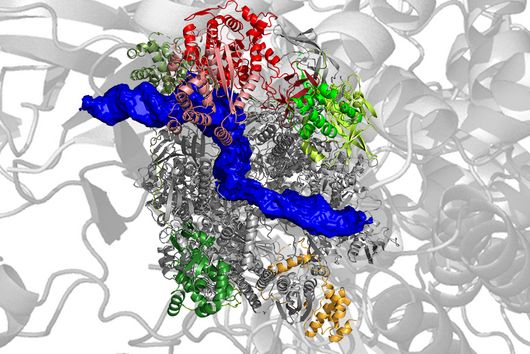
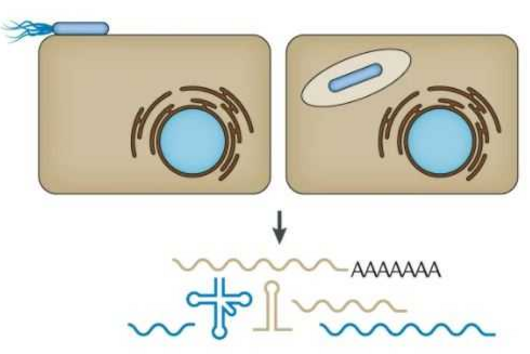
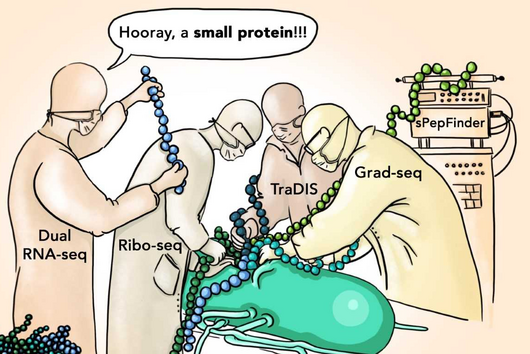
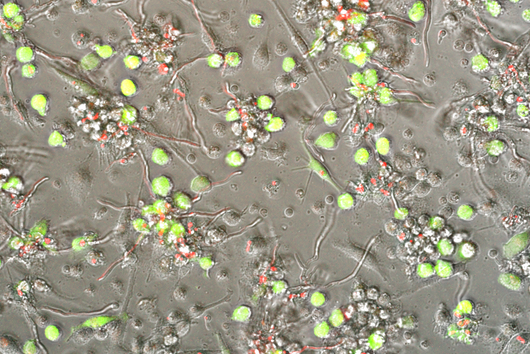
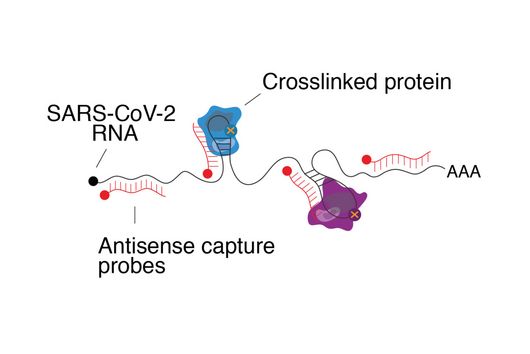
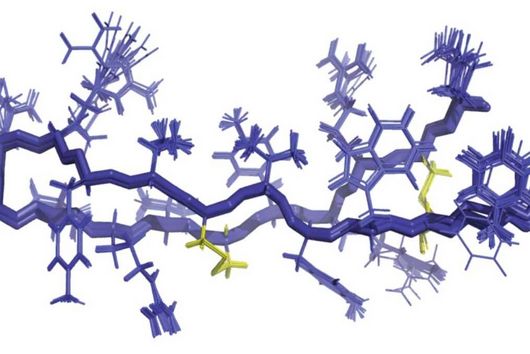
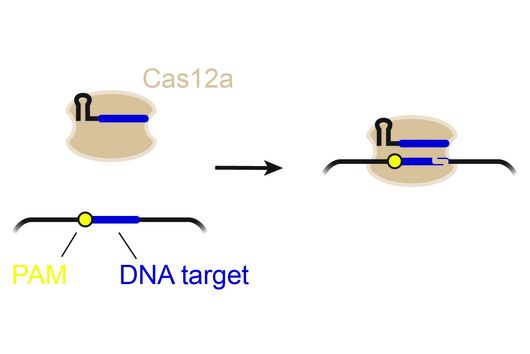
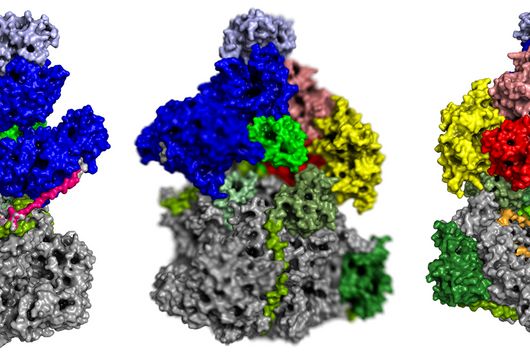
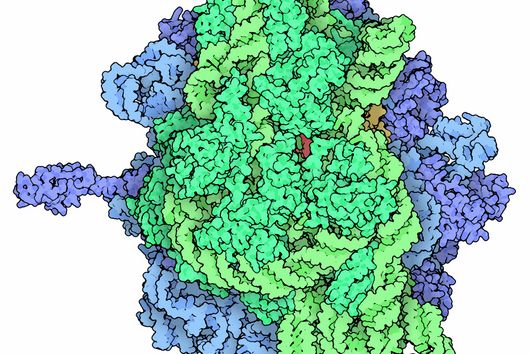
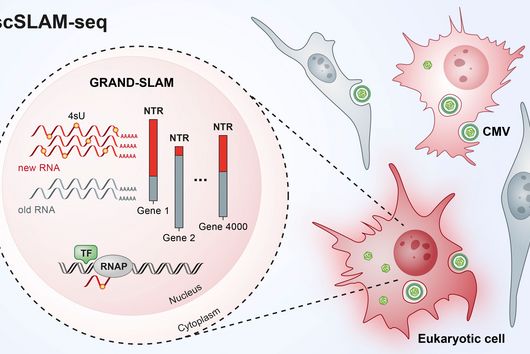
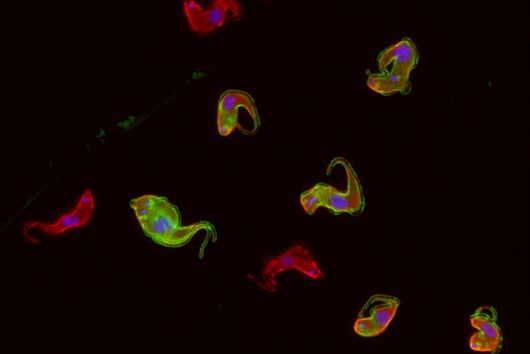
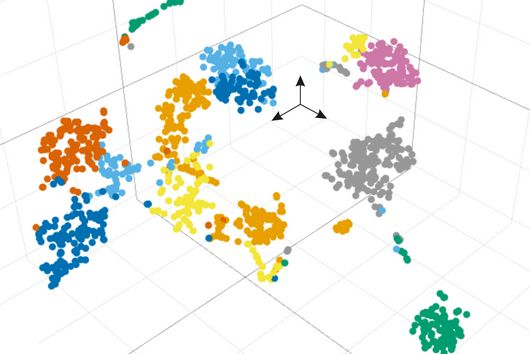
The investigations involved single-cell OMICs technologies, a collective term for modern laboratory methods that can be used to determine, for example, the gene activity and the amount of proteins on the level of individual cells – and thus with very high resolution. Using this data, the scientists characterised the properties of immune cells in the blood – the white blood cells. "By applying bioinformatics methods on this extremely comprehensive data collection of the gene activity of each individual cell, we could gain a comprehensive insight of the ongoing processes in the white blood cells," says Yang Li, Professor at the Centre for Individualised Infection Medicine (CiiM) in Hannover, a site of the Helmholtz Centre for Infection Research (HZI). Yang Li and her team brought their computational expertise and experience of single cell transcriptome analysis to this project.
"In combination with the observation of important proteins on the surface of immune cells, we were able to decipher the changes in the immune system of patients with COVID-19," adds Birgit Sawitzki, Professor at the Institute of Medical Immunology on Campus Virchow-Klinikum.
"Immature" cells
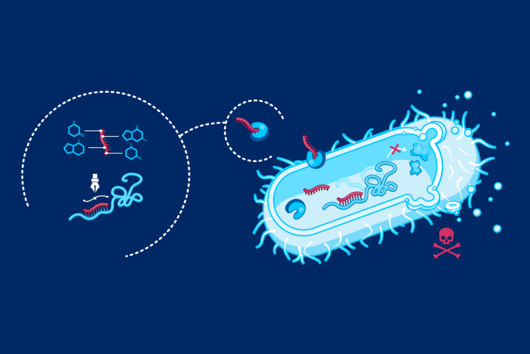
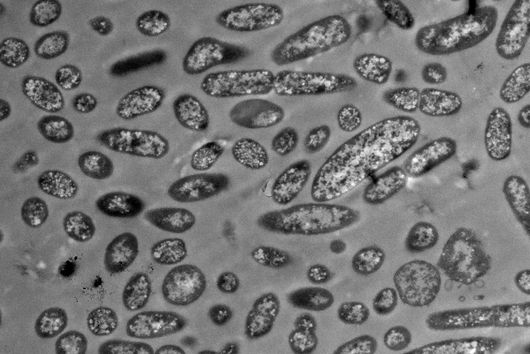
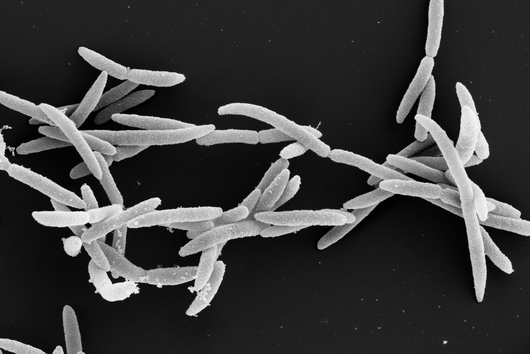
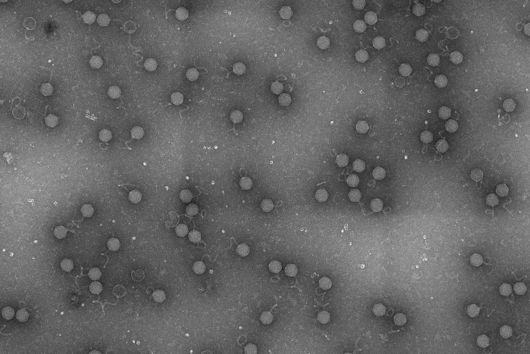
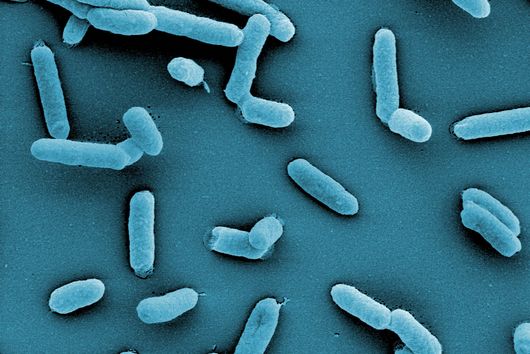
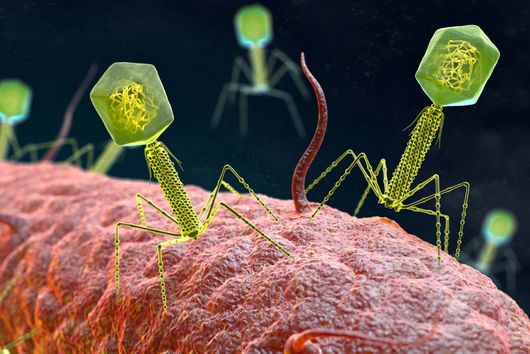
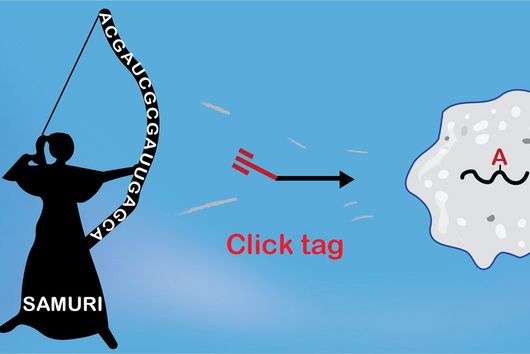
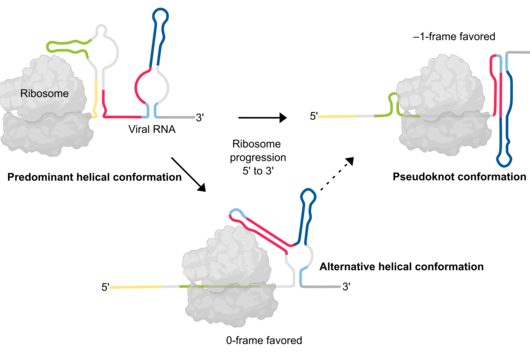
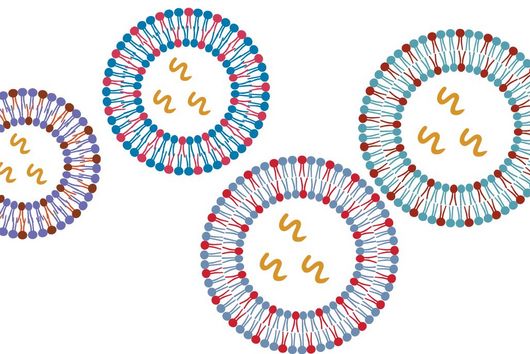
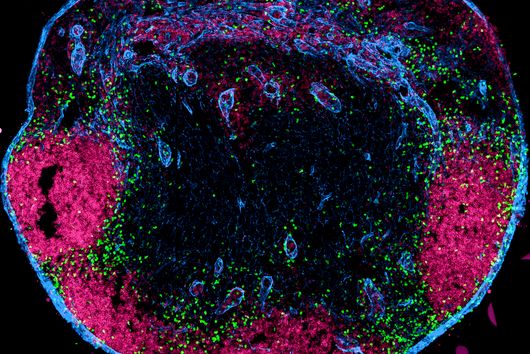
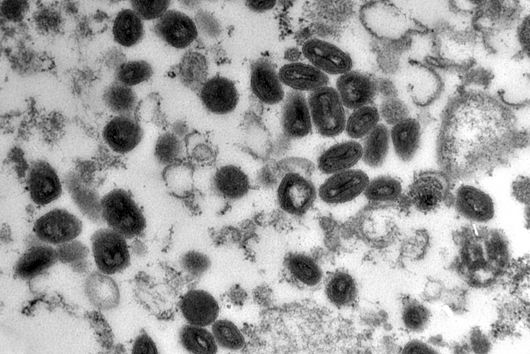
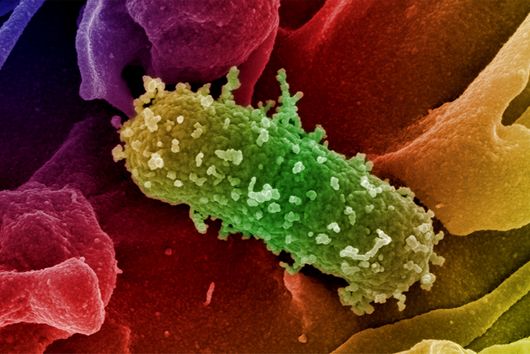
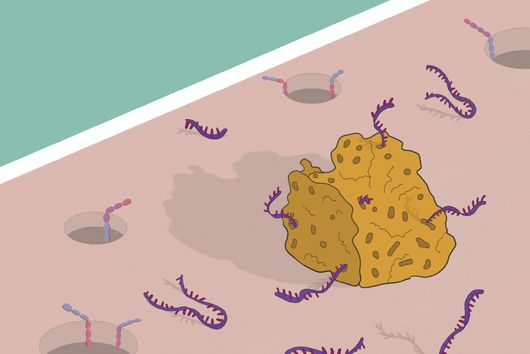
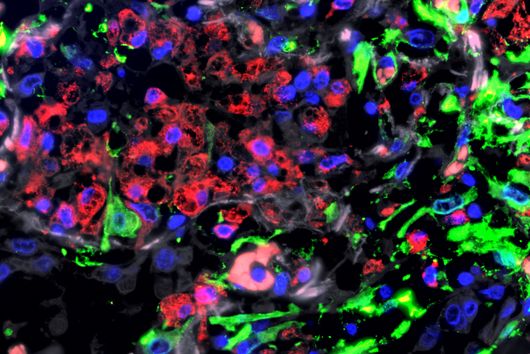
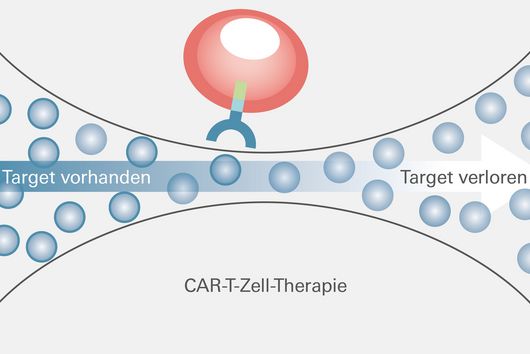
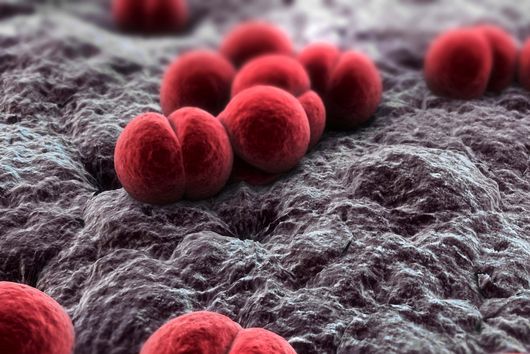
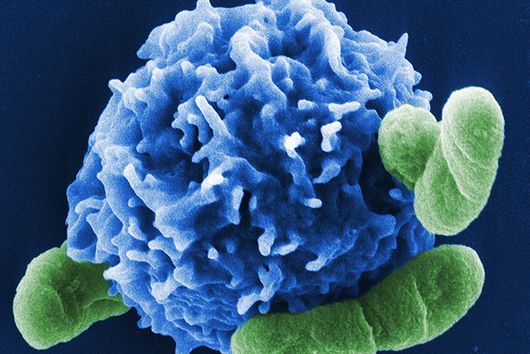
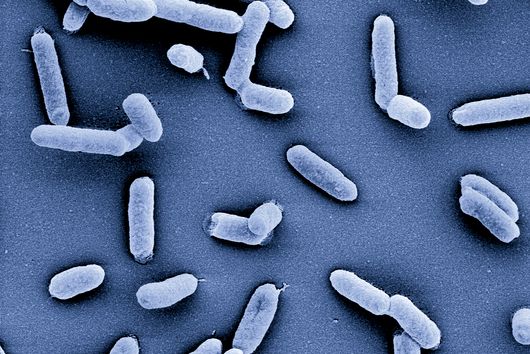
The human immune system comprises a broad arsenal of cells and other defense mechanisms that closely interact with each other. The current study focused on the so-called myeloid cells, which include neutrophils and monocytes. These are immune cells that are at the forefront of the immune response, i.e. they are mobilised at a very early stage to defend against infections. These cells also impact subsequent responses including the later formation of antibodies and other cells that contribute to immunity, placing the myeloid cells in a key position.
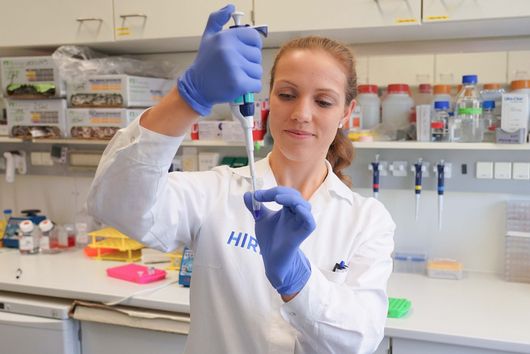
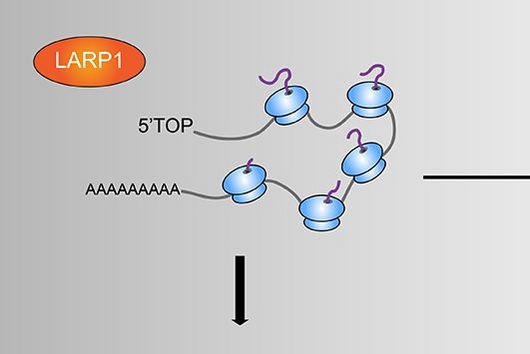
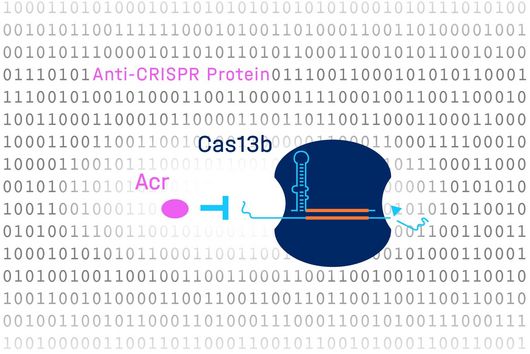
"With the so-called neutrophils and the monocytes we have found that these immune cells are activated, i.e. ready to defend the patient against COVID-19 in the case of mild disease courses. They are also programmed to activate the rest of the immune system. This ultimately leads to an effective immune response against the virus," says Antoine-Emmanuel Saliba, head of a research group at the Helmholtz Institute for RNA-based Infection Research (HIRI) in Würzburg, another site of the HZI.
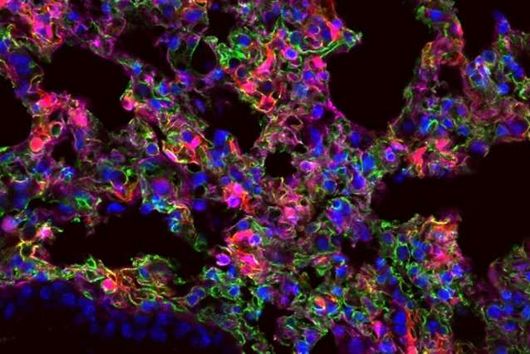
In contrast, the situation is different in severe cases of COVID-19, explains Sawitzki: "Here, neutrophils and monocytes are only partially activated and they do not function properly. We find considerably more immature cells that have a rather inhibitory effect on the immune response." Sander adds: "This phenomenon can also be observed in other severe infections, although the reason for this is unclear. The findings indicate that the immune system stands in its own way during severe courses of COVID-19. This possibly leads to an insufficient immune response against the coronavirus, while severe inflammation in the lung tissue proceeds.“
Approaches to therapy?
The current findings could point to new therapeutic options, says Anna Aschenbrenner from the LIMES Institute at the University of Bonn: "Our data suggest that in severe cases of COVID-19, strategies should be considered that go beyond the treatment of other viral diseases." The Bonn researcher says that in the case of viral infections one does not actually want to suppress the immune system. "If, however, there are too many dysfunctional immune cells, as our study shows, then one would very much like to suppress or reprogram such cells."
Jacob Nattermann, Professor at the Medical Clinic I of the University Hospital Bonn and head of a research group at the DZIF, further explains: "Drugs that act on the immune system might be able to help. But this is a delicate balancing act. After all, it’s not a matter of shutting down the immune system completely, but only those cells that slow down themselves, so to speak. In this case, these are the immature cells. Possibly, we can learn from cancer research. There is experience with therapies that target these cells."
Nationwide team effort
In view of the many people involved, Schultze emphasises the cooperation within the research consortium: "As far as we know, this study is one of the most comprehensive studies to date on the immune response in COVID-19 based on single cell data. The parallel analysis of two independent patient cohorts is one of the strengths of our study. We analysed patient cohorts from two different sites using different methods and were thus able to validate our findings directly. This is only possible if research data is shared openly and cooperation is based on trust. This is extremely important, especially in the current crisis situation.“
Original publication
Schulte-Schrepping et al.: Severe COVID-19 is marked by a dysregulated myeloid cell compartment. Cell (2020), DOI: 10.1016/j.cell.2020.08.001